3-minute read
In healthcare, outcomes aren’t just shaped in the doctor’s office—they’re shaped at home, at work, and in the communities where patients live. That’s why Social Determinants of Health (SDOH) are no longer optional—they’re central to empowering patients, delivering quality care, and reducing costs.
The Centers for Medicare and Medicaid (CMS) mandated that healthcare organizations track SDOH data for inpatients in 2024, and new mandates require it for outpatients in 2026. If you’re not ready to track, report, and act on SDOH data for outpatient populations by 2026, your organization will feel it—clinically, operationally, and financially.
Preparing for the Next Wave of SDOH Data Tracking
According to the World Health Organization, up to 30-55% of health outcomes are driven by non-clinical factors. This is why CMS requires healthcare organizations to screen inpatients for SDOH factors like food insecurity, housing instability, and transportation access, as well as refer patients to community organizations that can help.
In 2026, they are expanding these mandates to include outpatients. If organizations aren’t set up to track, report, and act on SDOH data, they will feel it—clinically, operationally, and financially.
Let’s Talk About Jane*
Jane is 55. She arrives at the ER with chest pain and undergoes surgery for a splint to help open up her artery. When the medical team discharges her, they prescribe heart meds and give her guidance for a healthier lifestyle with dietary and exercise recommendations.
But no one knows that she lives in a food desert, depends on a convenience store for her meals, can’t get to the pharmacy, and feels unsafe walking outside in her neighborhood for exercise. Three months later, she’s back in the ER, in worse shape, and the cost of care has increased.
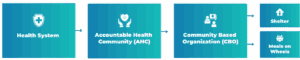
Now, imagine a system where they knew what Jane needed and connected her to the right community support for her non-medical needs. That’s one of the goals of the CMS’s SDOH mandates, and that is happening more as organizations incorporate SDOH into their inpatient care.
But here’s the thing: most systems aren’t built to make that referral meaningful. They can’t follow up, track outcomes, or close the loop. The referring hospital never knows if Jane got the resources she needed or if they impacted her health.
The Real Challenge: Data That Doesn’t Talk
The healthcare industry runs on data and is on a journey to make it work harder and smarter. But when you combine EHRs, community organizations, surveys, and care teams all speaking a different language, things get more complicated, and the intent and care break down.
In addition, traditional healthcare data standards weren’t built for Medicaid populations. These individuals may not have a home address or even a Social Security number. When hospitals try to apply conventional data fields, the system fails fast. And as data flows to partners, it breaks down even further because basic terminology doesn’t align. One system codes “homeless,” another says “unhoused.” The result: fragmented data, broken continuity of care, and missed opportunities to drive impact.
Today, SDOH data flows one way. Hospitals make a referral, and just like Jane’s case, they don’t hear back. There’s no follow-up, no accountability, and no insight into whether the intervention helped.
A one-way flow of data is not sustainable—not for patients, and not for the bottom line for payers and health systems.
Getting Ready for 2026: Outpatient Data
By 2026, CMS will require SDOH tracking for this population, and the volume of data will explode. If your team isn’t ready, you won’t just be behind—you’ll be missing real opportunities to improve care, cut costs, and comply with evolving regulations.
But there’s a solution. The Gravity Project – a collaborative effort to develop consensus-based data standards for SDOH- has contributed to USCDI (United States Core Data for Interoperability) for specific data elements that should be shared and FHIR (Fast Healthcare Interoperability Resources) for technical framework and implementation guides. Health systems adopting these standards with their community partners will finally be able to track referrals, measure impact, and prove value. To do this, they need to take steps to implement the standards and maintain them.
The Azulity team is healthcare-focused, outcome-driven
From cleansing and mapping your data to aligning with national standards and building governance models, we can help you put your SDOH data to work.
We are a data management consulting and implementation firm focused squarely and deeply on the healthcare space. Our team understands your challenges. We’ve been in your shoes, and we help our clients – payers and providers – overcome SDOH data obstacles. We can help you get your data ready for the next wave of SDOH data.
Check out the other parts of this series:
- Part 2: Don’t Drop the Data: The Impact of Completing the SDOH Data Loop
- Part 3: Turning SDOH Data into Measurable Impact
*Jane’s story is hypothetical for illustrative purposes
Chad Baker
Senior Customer Success Manager
 Chad Baker is an experienced manager with a proven ability to lead IT initiatives that positively impact diverse business teams and large customer bases. He has been involved in all phases of the development life cycle and has successfully managed technical teams under challenging timelines and aggressive targets. He is also well-versed in enhancing data maturity and lifecycle management.
Chad Baker is an experienced manager with a proven ability to lead IT initiatives that positively impact diverse business teams and large customer bases. He has been involved in all phases of the development life cycle and has successfully managed technical teams under challenging timelines and aggressive targets. He is also well-versed in enhancing data maturity and lifecycle management.
